Nipple discharge
It is the release of any fluid from the nipple of breast, and it is a common presenting symptom among women. [1]
The reported incidence of discharge from the nipple as a symptom of breast disease of all types varies from 5 to 10 per cent. Beasley stated that dis- charge can be milked from at least 90 per cent of apparently normal breasts, while Jackson and associates were able to obtain secretions from43 percent of patients having some type of complaint referable to the breast. [2]
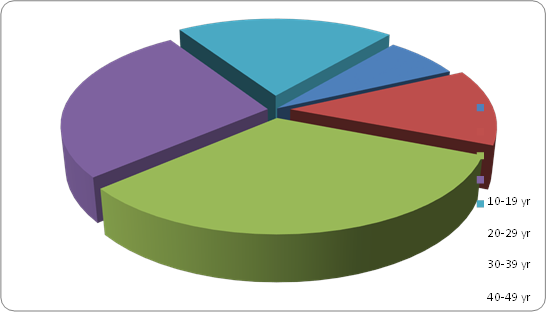
Age. The average ages of patients reported in most series were in the forties. River found the average age of 52 patients with discharge from the nipple to be 40.2 years, with range from 17 to 78 years. In the group having bloody discharge who were studied by Fits, Maxwell and Horn. [3]
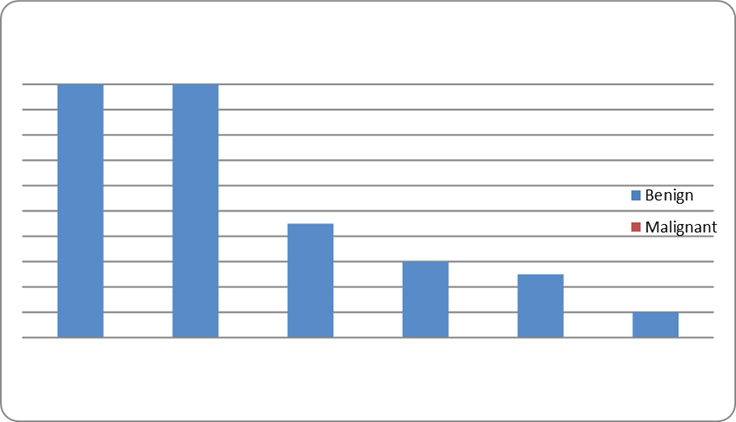
The average age of those with benign disease was 42years, and of those with carcinoma 54 years. In 59 cases of intraductal papilloma, Chester and Bell found an average ageof 49.4 years with range from 29 to 80 years. [4].
The breast is a group of large glands derived from the epidermis. It lies in a network of fascia derived from the dermis and the superficial fascia of the ventral surface of the thorax. The nipple itself is a local proliferation of the stratum spinosum of the epidermis. [5]
The mature breast of the female extends from the level of the second or third rib to inframammary fold at approximately the sixth or seventh rib. Transversely, it extends from the lateral border of sternum to the anterior axillary or midaxillary line. The axillary tail (of spence) extends superolaterally into the anterior axillary fold. The upper half of the breast, and particularly the upper outer quadrant, contains a greater volume of glandular tissue than do other sectors. [6]
The resting breast is defined as a postpubertal breast in an inactive state, not stimulated to become secretory by adequate hormone levels. The lactiferous sinus constitutes a lobe, with numerous lobules per lobe. It develops as a downgrowth of surface epithelium. Growth continues through the dermal papillary layer and into the reticular layer as the duct system is formed. [7]
Milk ejection occurs only during nursing. The sucking stimulation of the breast sends neural impulses to the hypothalamus. The hypothalamus stimulates oxytocin secretion by paraventricular nuclei cells, and suppresses the release of prolactin-inhibiting hormone (PIH). Oxytocin stimulates myoepithelial cells of secretory alveoli of the breast, effecting milk passage through the lactiferous ducts. Prolactin secretion is maintained when the PIH is suppressed and lactation continues. [8]
The diagnosis of ND begins with its characterization as either a physiological or pathological condition. Physiological discharge, often a manifestation of breast manipulation, is usually bilateral, is white or green, and emanates from many ducts [9].
A pathological discharge is generally unilateral, spontaneous, persistent, clear, watery, serous or bloody in appearance, and emanates from a single duct [10].
The nipple, which is well innervated by the 4th intercostal nerve, is surrounded by the areola. The pigmentation of the areola increases with pregnancy. Within the nipple and areola are some dermal papillae, and a very thin epithelium. [11]
Approximately 20 ducts open onto the surface of each nipple. The main ducts are called the lactiferous ducts. Stratified squamous keratinizing cells make up the epithelium of the ducts near their surface. Deeper in the ducts, the epithelium becomes a double layer of columnar cells. Smooth muscle is embedded within the dense connective tissue which supports the parenchymatous tissue. [8].
Some muscle is oriented circularly around the ducts; other muscle is longitudinally parallel with the ducts. Lactiferous sinuses are the dilated terminal portions of the lactiferous ducts, capable of storing milk during milk ejection. [8].
Due to loss of the placenta at birth, nipples can suffer from estrogen deficiency for a transient period until the ovaries increase hormone production. [12].
Dermis tissue surrounding the duct system is more cellular than in typical dermis and becomes the intralobular connective tissue. Less cellular dermis forms a coarser tissue which separates the lobules; it is thus interlobular connective tissue, with regions of adipose tissue contained within it. Some of the larger of these interlobular support structures form the suspensory ligaments (of Cooper). [13].
Intralobular ducts are lined with cuboidal epithelium: narrower ones have a simple cuboidal epithelium, larger ones a double layer of cuboidal epithelium. [14].
With pregnancy, the duct system completes its development. Many intralobular ducts form extensively during the proliferative phase. Secretory alveoli form at the tip of the smallest intralobular ducts and complete the lobules. Each secretory alveolus forms a small cul de sac (secretory lobule) lined with columnar epithelium. Myoepithelial cells are related to the basal side of each secretory alveolus. [8].
The secretory phase is brought on by changed levels of progesterone, lactogenic hormones (maternal and placental), and estrogen. Colostrum is secreted during the third trimester, milk shortly after birth. Not all lobules secrete at the same level. Therefore, under the microscope some lobules are distended, others are not. [12].
Interlobular partitions of connective tissue become considerably thinned as the secretory portions of the breast become more active and enlarged. Secretory cells produce numerous lipid droplets of widely varying sizes. [15]. While intracellular, lipid droplets are not surrounded by a membrane, but during exocytosis, they become enwrapped by cell membrane. Electron-dense secretory granules containing milk proteins also are found in secretory cells. These, too, undergo exocytosis. Columnar cells with sparse populations of microvilli are another component of secretory lobules. [15].
Nipple discharge
Most cases of ND are physiological in nature and are multi-ductal in origin. In these instances and particularly when associated with a creamy yellow, white or green coloured discharge, further investigations are rarely required.The term pathological nipple discharge (PND) has been introduced to describe a bloody, serous or clear discharge which is spontaneous,unilateral, uniductal and persistent. [16].
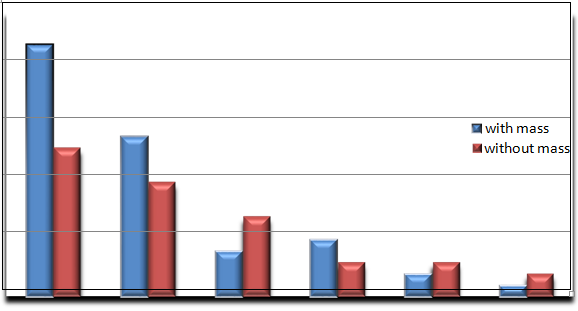
Discharge can occur from one or more lactiferous ducts.Management depends on the presence of a lump (which should always be given priority in diagnosis and treatment) and the presence of blood in the discharge or discharge from a single duct. Mammography is rarely useful except to exclude an underlying impalpable mass. Cytology may reveal malignant cells but a negative result does not exclude a carcinoma or in situ disease. [17].
A clear, serous discharge may be ‘physiological’ in a parous woman or may be associated with a duct papilloma or mammary dysplasia. Multiduct, multicoloured discharge is physiological and the patient may be reassured. [17].
A blood-stained discharge may be caused by duct ectasia,a duct papilloma or carcinoma. A duct papilloma is usually single and situated in one of the larger lactiferous ducts; it is sometimes associated with a cystic swelling beneath theareola. [17].
- A black or green discharge is usually the result of duct ectasia and its complications [17].
The important characteristics of the discharge and some other factors to be evaluated by history and physical examination are as follows:
Nature of the discharge (serous, bloody, or other), association with a mass, unilateral or bilateral, single or multiple duct discharge, discharge is spontaneous (persistent or intermittent) or must be expressed, discharge is produced by pressure at a single site or by general pressure on the breast, relation to menses, premenopausal or postmenopausal, and patient is taking contraceptive pills or estrogen. [8].
Spontaneous, unilateral, serous, or serosanguineous discharge from a single duct is usually caused by an intraductal papilloma or, rarely, by an intraductal cancer. A mass may not be palpable. The involved duct may be identified by pressure at different sites around the nipple at the margin of the areola. Bloody discharge is suggestive of cancer but is more often caused by a benign papilloma in the duct. [18].
Cytologic examination may identify malignant cells, but negative findings do not rule out cancer, which is more likely in women over age 50 years. In any case, the involved duct—and a mass if present—should be excised. A ductogram (a mammogram of a duct after radiopaque dye has been injected) is of limited value, since excision of the suspicious ductal system is indicated regardless of findings. Ductoscopy, evaluation of the ductal system with a small scope inserted through the nipple, has been attempted but is not effective management. [18].
In premenopausal women, spontaneous multiple duct discharge, unilateral or bilateral, most noticeable just before menstruation, is often due to fibrocystic condition. Discharge may be green or brownish. Papillomatosis and ductal ectasia are usually detected only by biopsy. If a mass is present, it should be removed. [19].
A milky discharge from multiple ducts in the nonlactating breast may occur from hyperprolactinemia. Serum prolactin levels should be obtained to search for a pituitary tumor. Thyroid-stimulating hormone (TSH) helps exclude causative hypothyroidism. Numerous antipsychotic drugs and other drugs may also cause a milky discharge that ceases on discontinuance of the medication. [19].
Oral contraceptive agents or estrogen replacement therapy may cause clear, serous, or milky discharge from a single duct, but multiple duct discharge is more common. In the premenopausal woman, the discharge is more evident just before menstruation and disappears on stopping the medication. If it does not stop, is from a single duct, and is copious, exploration should be performed, since this may be a sign of cancer. [12].
Hormonal shifts from sexual stimulation, pituitary tumors, and the use of certain medications like birth control pills, blood pressure medications, major tranquilizers, antidepressants, or ulcer medications can cause an imbalance in the hormone prolactin which stimulates milk production.
Breast Infection: A spontaneous pus-like discharge from the nipple due to a mastitis (breast infection) or breast abscess and may require an antibiotic to treat. [12].
Duct ectasia: Multi-colored discharge from one nipple that occurs most often in a milk duct that is clogged and swollen. Although it usually clears up by itself, it should be monitored. [12].
Intraductal papilloma: This is a small benign (not cancer) wart-like growth in a duct lining near the nipple, which may become irritated and bleed, producing a pinkish, brown or bloody discharge. It is the most common cause of bloody nipple discharge and should be removed. [12].
History of breastfeeding: Galactorrhea is a term used to describe a milky discharge from both breasts. It occurs most often in non-breastfeeding women after pregnancy and can last a year or two. [12].
Stimulation: Squeezing or expressing the breast or nipple can produce a nipple discharge.
Fibrocystic breast changes: Cysts (sacs filled with fluid) and changes in the fibrous tissue of the breast can cause nipple discharge that is often greenish. [12].
Breast cancer: This can very rarely cause a bloody or clear nipple discharge. [12].
Workup
The standard workup for patients presenting with nipple discharge includes a thorough history and physical examination in addition to a complete breast imaging evaluation. Imaging studies allow potential localization and characterization of the lesion in question, with the option of percutaneous image-guided biopsy to achieve a tissue diagnosis. [20]. Typically, mammography and ultrasound are used to identify mass lesions responsible for nipple discharge. Additionally, magnetic resonance imaging (MRI) may be useful in the workup of pathologic nipple discharge when lesions cannot be localized with mammography or ultrasound. [20]. While MRI has been preliminarily studied for this indication at a few centers, it is not generally part of the workup. When nipple discharge is determined to be of benign etiology, duct excision may also be indicated to eliminate discharge when bothersome to the patient. [21].
In the absence of a mass or other lesion identified with breast imaging, the conventional surgical approach has been to perform major duct or lacrimal probe-guided excision. However, a histopathologic etiology is not always found on major duct or lacrimal probe-guided excision, which raises the possibility that the causative lesion might have been left in situ. [21]. Diagnostic ductography allows preoperative determination of the number, location, and extent of any underlying lesions. Preoperative use of ductography with methylene blue injection to localize lesions has been shown to increase the likelihood that a specific pathologic lesion will be found at surgery. [22] Ultrasound imaging uses high frequency sound waves to produce a picture of the internal structures of the breast. A small handheld probe is pressed gently against the skin surface. It both generates inaudible sound waves and detects any echoes reflected back off the surfaces and tissue boundaries within the breast. [23] From these reflected sound waves the computer generates a real time picture which is displayed on the monitor. The probe is moved across the skin to view the breast from different angles. Breast ultrasound is used to help clarify breast abnormalities felt by a doctor during a physical examination and to characterize potential abnormalities identified on mammography. [24]. Ultrasound is particularly good at determining if a lump is solid (which may be a non-cancerous lump or a cancerous tumour) or fluid-filled (such as a benign cyst). Ultrasound is also used to guide aspiration or biopsy of a lump.
[24]. Mammography is a specific type of imaging that uses a low-dose x-ray system to examine breasts. A mammography exam, called a mammogram, is used to aid in the early detection and diagnosis of breast diseases in women. [25].
An x-ray (radiograph) is a noninvasive medical test that helps physicians diagnose and treat medical conditions. Imaging with x-rays involves exposing a part of the body to a small dose of ionizing radiation to produce pictures of the inside of the body. X-rays are the oldest and most frequently used form of medical imaging.Three recent advances in mammography include digital mammography,computer-aided detection and breast tomosynthesis. [26]. Digital mammography, also called full-field digital mammography (FFDM), is a mammography system in which the x-ray film is replaced by solid-state detectors that convert x-rays into electrical signals. These detectors are similar to those found in digital cameras. The electrical signals are used to produce images of the breast that can be seen on a computer screen or printed on special film similar to conventional mammograms. From the patient's point of view, having a digital mammogram is essentially the same as having a conventional film mammogram. [25]. Computer-aided detection (CAD) systems use a digitized mammographic image that can be obtained from either a conventional film mammogram or a digitally acquired mammogram. The computer softwa3re then searches for abnormal areas of density, mass, or calcification that may indicate the presence of cancer. The CAD system highlights these areas on the images, alerting the radiologist to the need for further analysis. [25]. Breast tomosynthesis, also called three-dimensional (3-D) breast imaging, is a mammography system. [27].
Where the x-ray tube moves in an arc over the breast during the exposure. It creates a series of thin slices through the breast that allow for improved detection of cancer and fewer patients recalled for additional imaging. [27]. Fine-needle aspiration (FNA) of the breast is an established diagnostic method in the evaluation of palpable breast masses. [28]. Its reliability has also been demonstrated in the diagnosis of radiologically imaged, nonpalpable lesions. [29]. Fine needle aspiration (FNA) cytology has been widely used for the diagnosis of palpable breast masses. [30]. The technique involves the insertion of a fine needle (between 21 and 25 gauge) into a lesion and the extraction of a small sample of cellular material which is smeared onto glass slides. [31]. The cells are stained and examined morphologically by cytopathologists. Fine needle aspiration is simple, fast, and can be performed as an office procedure, since it requires no special equipment, causes minimal morbidity, and has high patient acceptance. [32].