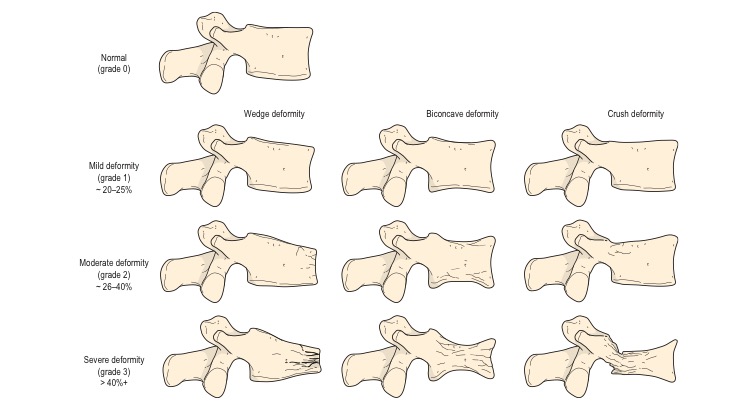
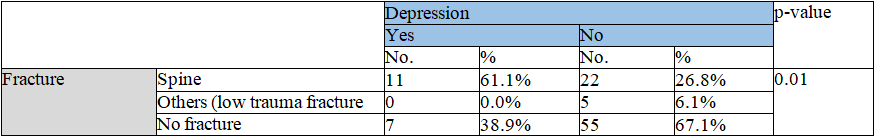
Osteoporosis is a medical condition that is characterized by a decrease in bone density and deterioration of the bone structure, resulting in increased vulnerability to fractures [1]. The issue at hand represents a significant public health concern, as it is linked to heightened rates of illness and death, specifically in relation to fractures occurring in the hip and vertebrae. These fractures place a substantial strain on the healthcare system due to the considerable financial expenses associated with their treatment and the resulting disabilities they give rise to (Al-Mukhtar et al., 2013) [2]. According to the World Health Organization (WHO), fractures are the primary clinical characteristic of osteoporosis. Osteoporotic fractures are characterized by being the result of trauma that would not typically produce a fracture in healthy bone. To clarify, a fragility fracture may occur as a consequence of little stress, such as a fall from a height equivalent to standing or lower [3]. The manifestation of vertebral fractures in a clinical setting includes symptoms such as back discomfort, restricted range of motion in the spine, reduction in height, and functional impairment. Individuals may have challenges in activities such as, climbing stairs, rising, bending, dressing as well as a decrease in walking speed, diminished independence, or reliance on assistive devices [4]. According to the cited source (Cauley et al., 2007) [5], the occurrence of vertebral fractures significantly amplifies the likelihood of subsequent vertebral fractures by a factor of four to five, as well as the risk of other fragility fractures by a factor of two to four. During the initial year following fracture, hip fractures have more pronounced functional, economic, and health-related implications compared to vertebral fractures. Nonetheless, in the long run, vertebral fractures have an equivalent impact in terms of extended mortality and diminished quality of life (QOL) [6]. Other common sites for fragility fractures are the distal radius, proximal humerus, ribs, pelvis, clavicle, femur and tibia [7]. The semi-quantitative grading (SQ) method is commonly utilized in epidemiology studies and pharmaceutical trials to determine the prevalence and incidence of vertebral fractures. This method is particularly prevalent in evaluating the effectiveness of new osteoporosis treatments (Figure 1) [8].
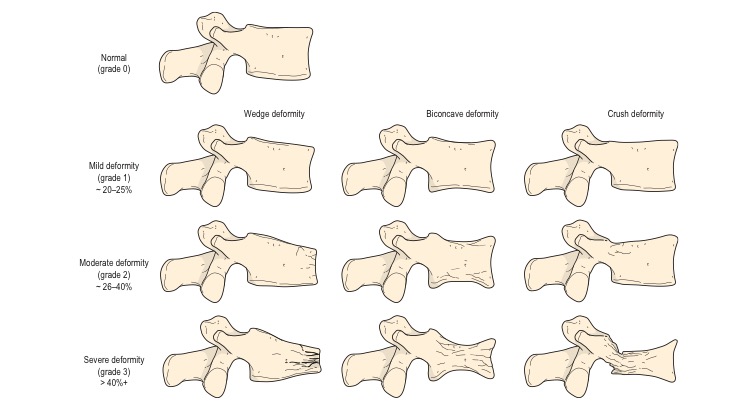
Figure 1: The semiquantitative method of grading of Genant et al.
Epidemiology
Osteoporosis is a significant concern within the realm of public health. According to the National Osteoporosis Foundation (NOF), it is estimated that osteoporosis affects around 10.2 million individuals in the United States, with an additional 43.4 million individuals having low bone mass. Annually, the United States experiences a prevalence of over 2 million fractures associated with osteoporosis, with a significant majority of these fractures, exceeding 70%, affecting the female population [9,10]. In Iraq the Prevalence of Osteoporosis in Post-Menopausal Iraqi Women was 22.8%. Distribution of the study sample was 65.6% for age group 50-60 years, 29.2% for age group 61-70 years, 5.2% for age group>70 years [11].
Risk factor
Numerous factors were recognized as contributing to the increased danger of osteoporosis and/or fragility fractures. Among these factors female gender and increasing age, stand out as particularly significant risk factors. However, additional prevalent and potentially modifiable risk factors encompass chronic inflammatory disease, long-term corticosteroid therapy, untreated premature menopause, and malabsorption and [12]. Numerous factors have been noted to be contributors to the heightened susceptibility to osteoporosis and/or fragility fractures. Among these factors, female gender and advancing age are recognized as particularly significant risk factors [13]. Nevertheless, additional prevalent and potentially modifiable risk factors involve chronic inflammatory disease, long-term corticosteroid therapy, and untreated premature menopause malabsorption. Estrogen deficiency induced imbalance between bone formation and resorption such that resorption predominates over formation [14].
Diagnosis
Dual-energy x-ray absorptiometry (DEXA) is the most applicable method to assess bone mineral density (BMD), it is highly accurate x-ray technique [15]. One significant benefit of Dual-energy X-ray absorptiometry (DEXA) is its ability to subject the patient to radiation levels that are roughly 90% lower compared to those of a conventional chest radiograph [16]. As per the standards established by the World Health Organisation (WHO), osteoporosis is characterised by a Bone Mineral Density (BMD) that falls 2.5 standard deviations (SD) or more below the mean value observed in young, healthy women (equivalent to a T score of less than -2.5 SD) [17]. The AACE concurs with the recommended clinical diagnosis put out by the National Bone Health Alliance, which suggests that osteoporosis may be diagnosed in individuals with osteopenia and a heightened risk of fractures by employing FRAX® country-specific criteria [18], appendix 1).Other diagnostic procedures include : high resolution peripheral quantitative computed tomography (HR-pQCT), quantitative computed tomography (QCT), quantitative ultrasonography , magnetic resonance imaging (MRI) and biochemical bone turnover markers (BTM) [19].
Treatment
Bisphosphonates are extensively utilised in pharmaceutical medication for the treatment of skeletal disease. Generally, these medications are well tolerated, with serious adverse events being rare. The risk-benefit profile in osteoporotic patients is overwhelmingly favourable, making them a preferable option [20]. While it is important to undergo appropriate bone mineral density screening and receive medication treatment, it is worth noting that osteoporosis can be prevented through proper management of diet, lifestyle, and interventions aimed at preventing falls [21].
Major depressive disorder (MDD)
This mental disorder is quite widespread, impacting around 16% of the adult population in the United States [22]. The incidence of major depressive episodes in the general population of Iraq was found to be 12% among individuals aged 50-64 years and 13% among those aged 65 years and above [23]. It is characterized by a sleep abnormality, anhedonia, sustained depressive mood, social behaviors, and alongside a number of motivational [24]. According to the World Health Organisation, severe depression has been identified as the primary contributor to global disability. Depression causes decreases life quality, suffering, and impairment in occupational and social functioning. The condition is associated with escalated healthcare expenditures, as well as elevated prevalence rates of several chronic medical ailments [25]. The presence of a depressed mood does not always indicate the presence of mental disorders. It is plausible that such a response may be considered within the realm of typical reactions to specific life circumstances, indicative of particular physiological ailments, or an outcome of pharmaceutical interventions or medical procedures.
Population-based clinical investigations have observed a higher occurrence of Major Depressive Disorder (MDD) during the perimenopausal phase in comparison to both the premenopausal and postmenopausal stages. The available evidence indicates a correlation between fluctuations and decline in hormone levels and the reported rise in risk for severe depressive illness [26].
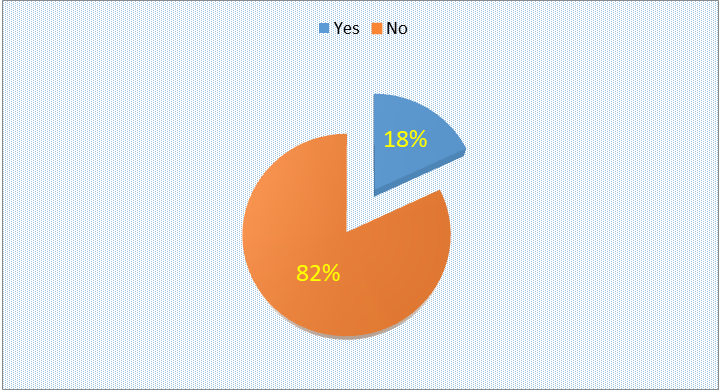
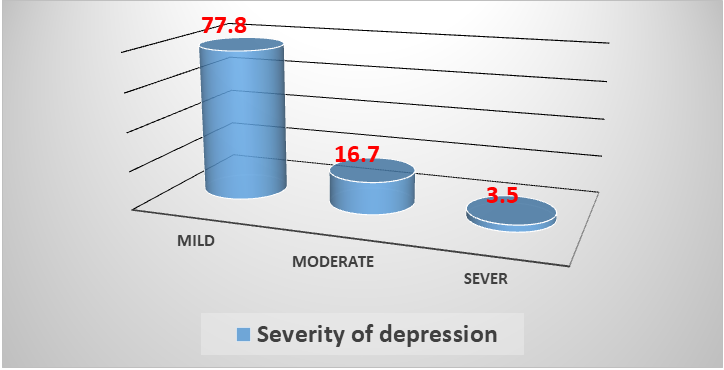
Osteoporosis and depression
The presence of osteoporosis can exert a substantial influence on the psychological well-being and health-related quality of life (HRQOL) of individuals. The initial recognition of the coexistence of depression among individuals diagnosed with osteoporosis was documented throughout the latter part of the 1980s through observational investigations conducted within the framework of osteoporosis educational initiatives. When queried about the origins of these despondent emotions, a significant number of participants expressed that the consequences of osteoporosis—chronic pain, failure to meet societal role expectations, deformity, and loss of control resulted in more negative feelings [27]. There is a lack of empirical data supporting a direct causal relationship between osteoporosis and psychological disorders, specifically depression [28]. Osteoporosis, in the absence of concurrent clinical fractures, has been linked to adverse outcomes such as impaired physical ability, deformity, chronic pain, depressed mood, poor well-being, loss of control, and reduced social activity, resulting in a diminished quality of life [29]. The findings of the Multiple Outcomes of Raloxifene Evaluation (MORE) study revealed a higher prevalence of depression in individuals diagnosed with osteoporosis. This association was particularly prominent in postmenopausal women with vertebral fractures, who exhibited a significantly greater occurrence of depressive symptoms and probable depression compared to those without fractures [30]. Fractures, especially vertebral fractures, can be associated with chronic, disabling pain; in addition, fractures can be extremely debilitating [31]. Up to our knowledge, there are no previous reports about Prevalence of Major Depressive Disorder Among postmenopausal Iraqi women with osteoporosis.