Study area- The study was conducted in Department of Ophthalmology, Indira Gandhi Medical College, Shimla, Himachal Pradesh.
Study period- The study was conducted for 12 months after approval from Institutional Ethics Committee from July 2018 to June 2019.
Study design- It was a cross-sectional descriptive study of diagnosed patients of Diabetes mellitus attending eye OPD of Indira Gandhi Medical College, Shimla, Himachal Pradesh.
Study population- Patients with Type II diabetes mellitus with and without fundus changes of Non-Proliferative Diabetic Retinopathy (NPDR) of any severity.
Selection Criteria
Inclusion criteria:
Patients with Type II Diabetes Mellitus on or off treatment within age group of 40-70 years reporting in the OPD after the start of the study.
Patients who gave their consent for participation in the study.
Exclusion criteria:
Patient with pre-existing macular pathology such as ARMD, hereditary maculopathy.
Patient who have undergone any laser surgery in retina.
Hypertensive retinopathy more than grade II.
Uveitis.
Media haze grade 3 or 4.
Patient who have undergone cataract surgery.
Patients with history of ocular trauma.
Patients with proliferative diabetic retinopathy.
Patients taking retino toxic drugs.
Type I Diabetes Mellitus.
Not willing for study.
Materials-After taking history each patientunderwent ophthalmic examination as given below:
For Visual acuity:
• Snellen’s chart for distant vision.
• Jaeger’s chart for near vision.
Refraction:
• To rule out any refractive error.
For Complete anterior segment examination:
•Slit Lamp Biomicroscopy (HAAG STREIT-BQ 900 WITH IMAGING MODULE IM 900 made in Switzerland) examination to see anyopacity in the media, lens for evidence of cataract, pseudophakia, aphakia and anterior vitreous for pigment and cells.
For Intra Ocular pressure:
• Schiotz tonometer/Goldmann’s applanation tonometer/NCT.
For Colour vision:
• Ishihara’s pseudo isochromatic plates
Amsler’s grid test for both eyes
For Fundus examination:The pupil was dilated by instilling one to two drops of 5% Phenylephrine Hydrochloride with 0.8% Tropicamide, in patients with normal IOP and normal anterior chamber depth. After 45 minutes when the pupil was fully dilated, the patient was examinedwith:
• Direct ophthalmoscope (HEINE Beta 200S)
• Volk’s +90 D aspheric lens under slit lamp
• Indirect ophthalmoscope (AAIO WIRELESS)
For Central macular thickness:
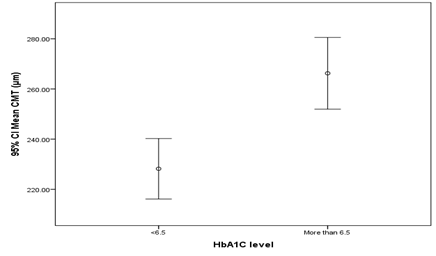
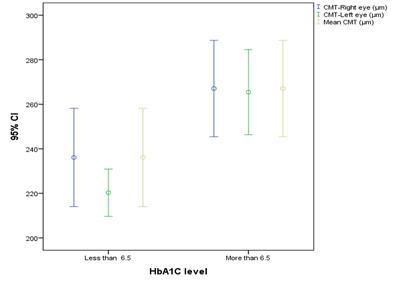
SD-OCT volume scan with TOPCON 3D OCT-1 Maestro (Version 8.42) under dilation with 5% Phenylephrine Hydrochloride with 0.8% Tropicamide in every patient. Using the retinal thickness map analysis protocol, macular thickness was determined and compared with normative data. It consists of a macular cube 512 × 128 (vertical × horizontal) axial scans covering an area of 6 × 6 mm in the macular region. The macula was divided into 3 concentric circles centered at the fovea. This division is a superimposition of the ETDRS map over the OCT map of the macula. It consists of 3 zones; the fovea (less than 1 mm diameter), the inner macula (1 to 3 mm) and the outer macula (3 to 6 mm).Foveal or central macular thickness is defined as the average thickness in the central 1 mm diameter. The central macular thickness was measured thrice and average was calculated.
Investigations:
The results of glycosylated haemoglobin (HbA1c) test, lipid profile and other relevant investigations done were recorded for each patient.