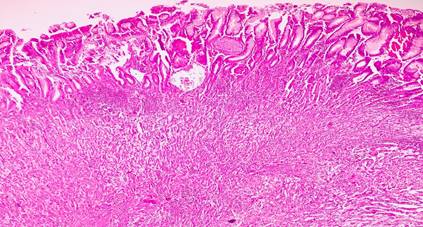
Hepatoid Adenocarcinoma (HAC) is a malignant tumor which resembles microscopic features of hepatcellular carcinoma, but occurs outside the liver. Hepatoid Adenocarcinoma of Stomach (HAS) is a rare tumor associated with poor prognosis [1]. According to Lauren’s classification HAS belongs to the indeterminate type of gastric carcinoma [2]. The pathological diagnosis of this tumor, is based on microscopic characteristics irrespective of serum Alpha Fetoprotein levels (AFP) or tissue AFP staining by Immunohistochemistry (IHC) [3,4].
Stomach is the most common location of HAC. The incidence of HAS is <1% [5]. Other sites for HAC include colon, lung, gall bladder, uterus, urinary bladder, etc. [6].
In the year 1985, Ishikura et al. first proposed this entity. Nagai et al suggested that HAC should be diagnosed on its morphological features and not on production of AFP levels [7,8].
HAS has a male to female ratio of 2.3:1. Mean age at the time of presentation is 63 years [5]. HAS is not associated with specific clinical features. Most symptoms include general fatigue, decreased appetite, epigastric pain, anemia, melena, etc. however, sometimes HAS, may present with gastric perforation [5]. Our patient presented with epigastric pain and weight loss. Wanget et al. reported that majority of HAS were located in gastric antrum (57%), followed by gastroesophageal junction and gastric body [9].
Most HAC are associated with production of AFP, but not all AFP producing carcinomas histologically show hepatoid features, Classically the tumors with elevated AFP levels are heptocellular carcinoma, hepatoblastoma, germ cell tumors (particularly Yolk sac tumor). Apart from them gastric cancer, lung cancer, renal cell carcinoma, nephroblastoma, pancreatic cancer, colorectal carcinoma, ovarian carcinoma and rhabdomyoblaastoma may also produce increased amount of AFP levels [10].
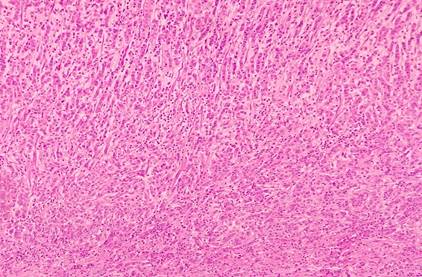
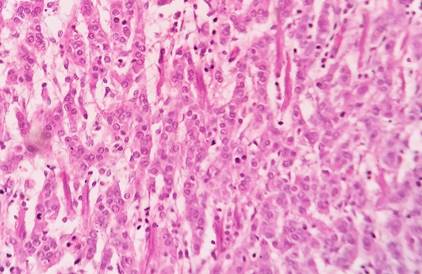
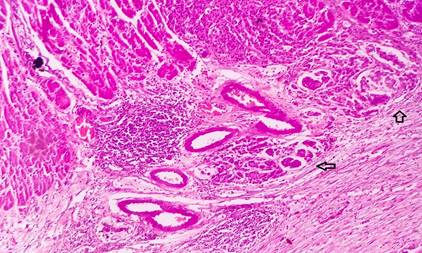
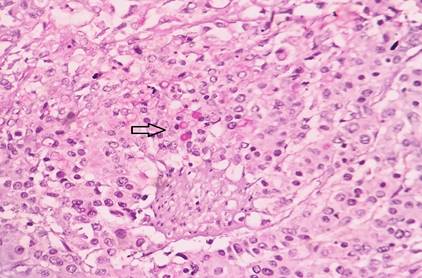
Kodama et al. described two histological types of HAS. The first was medullary type, characterized by solid nests ans sheets of polygonal cells. Along with scattered large pleomorphic or multinucleate giant cells. The second, being well differentiated papillary or tubular type with clear cytoplasm. Both the types can sometimes coexist in the same tumor [6]. The tumor cells, invade the surrounding tissue and are accompanied by significant venous infilteration [5].
Therefore HAC, should be diagnosed by characteristic histological features of a gastric tumor resembling hepatocellular carcinoma, distinction between HAS and ALP producing gastric cancer is necessary as HAS carry a dismal prognosis [4].
Only a minority of a HAC, show more definitive features of hepatoid differentiation like bile production, intracytoplasmic pale bodies and albumin m RNA production [10]. Presence of PAS positive diastase resistant intracytoplasmic eosinophilic granules is a non-specific finding but can be supportive of diagnosis [10]. About 9.7% cases can show hyaline globules [11].
Our case had characteristic tumor cell morphology, along with increased production of AFP levels, presence of pale bodies and PAS positive diastase resistant hyaline globules.
Most common sites of metastasis of HAS include lymph node (77%) and liver (42%), followed by lung, peritoneum, pancreas, spleen and brain [11].
On IHC, this tumor shows reactivity for AFP, Alpha antitrypsin, Alpha Chymotrypsin, CarcinoEmbryonic Antigen [12].
HAS carries a poor prognosis as compared to gastric adenocarcinoma with no hepatoid features regardless of AFP production. About 5 year survival rate is about 9% [12].