Study area
The study was conducted in Sokoto metropolis. Sokoto metropolis lies between longitudes 0.5°.11’ to 13°.03’ east and latitude 13°.00 to 13°.06 north [12]. Sokoto State is at the extreme part of North-western region of Nigeria, sharing a border with Niger Republic to the North with a total land area of 32,000 square kilometers and a population of 4,602,298 million. There are two seasons in Sokoto; the dry season and the raining seasons in which the harmattan season ranges from October to February [13] Farming and animal husbandry are the major occupation in this region, comprising of Hausa and Fulani [14].
Study Population and Design
This descriptive study was conducted at the infectious diseases clinic among HIV seropositive patients 18 years and above that visited Usmanu Danfodiyo University Teaching Hospital (UDUTH), Sokoto, Sokoto State, Nigeria by analyzing the serum samples collected. At the clinic an average of 10 to 20 HIV patients are seen daily and between 25 to 70 patients are seen weekly including male and female patients from different works of life. And their CD4+ cells are monitored too.
Ethical Considerations
The participants gave their written informed consent before they were enrolled in the study. All data were analyzed anonymously throughout the study. Ethical approval was obtained from the UDUTH Health Research Ethics Committee Sokoto (UDUTH/HREC/2021 /1052/V3) and Sokoto State Ministry of Health (SKHREC/068/2021).
Inclusion and Exclusion Criteria
All HIV seropositive patients (male and female) attending IDC of UDUTH Sokoto, Sokoto State, who gave written informed consent to participate in the study was included in the study. Non HIV, non-adult and patients who did not give written informed consent to participate in the study were excluded.
Sample Size Determination
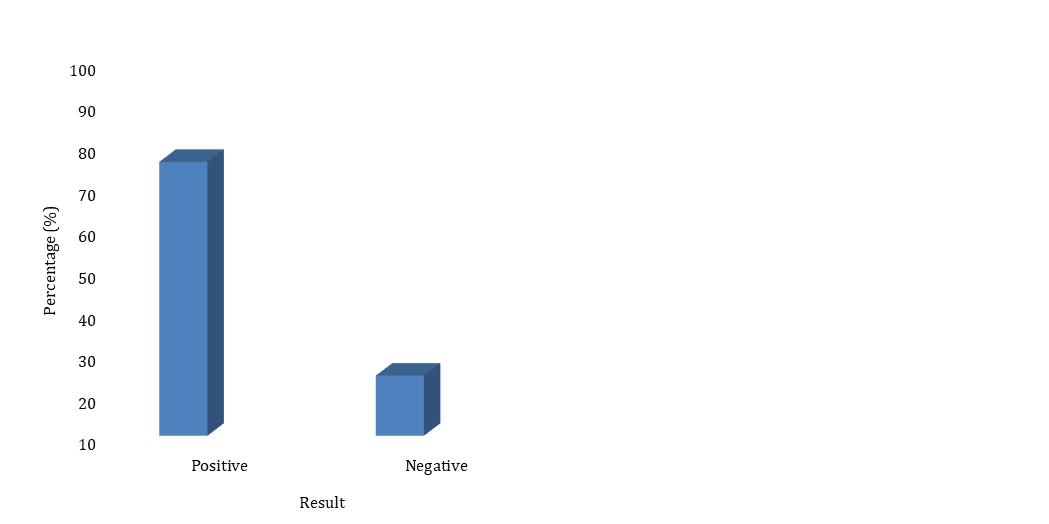
Sample size was estimated using fisher’s formula [15] adopting a prevalence rate of 45.4 % [9] as follows; N = Z2pq/d2 where ‘N’ is the required sample size, ‘Z’ is the confidence interval at 95% (1.96), ‘p’ is estimated prevalence from previous studies = 45.4 % , ‘q’ is 1 – p, and ‘d’ is the degree of accuracy set at 0.05.Substituting; N= 1.962 x 0.454 x 0.546/0.052 and this gives a sample size of 381.
Sample Collection and Analysis
Patients were consecutively recruited after giving informed consents. Five (5) ml amount of whole blood samples was collected aseptically into two (2) ml amount of ethylenediaminetetraacetic (EDTA) acid-preserved blood sample bottle and was spun at 12000/g for 10 minutes to harvest their serum samples for HTLV-1/2 serological tests. HIV surface antigen was determined using HIV Test Strip (determine kit). The foil of the strip was pilled off and placed on the bench top then a drop of serum sample was placed on the sample pad on the strip using a pasteur pipette. The strip was allowed to stand for 15 minutes. Then the result was read. Anti-HTLV IgM and IgG antibodies in serum of HIV-1 patients were determined by HTLV-1+2 ELISA Test Kits (Nanjing Pars Biochem, China).
Determination of HIV Surface Antigen Using HIV Test Strip (Determine HIV Early Detect)
The foil of the strip was pilled off and placed on the bench top then a drop of serum sample was placed on the sample pad on the strip using a pasteur pipette. The strip was allowed to stand for 15 minutes. Then the result was read (Abbott Diagnostic Medical Co. Ltd, Matsudo, Japan).
Determination of anti–HTLV IgM and IgG antibodies in serum of HIV patients
Analysis of IgG and IgM Antibodies to HTLV were detected using human T–lymphotrophic virus sandwich ELISA. The micro–ELISA strip plates were pre–coated with an antigen specific to HTLV IgG and IgM antibodies respectively. Standards test samples were added to appropriate micro–ELISA strip plate wells and combined to specific antigen. Then a horseradish peroxidase (HRP)-conjugated antigen specific to HTLV was added to each micro-ELISA strip plate well and incubated. Free components were washed away. The TetraMethylBenzidine (TMB) contained HTLV substrate solution was added to each well. Only those wells that contained HTLV-IgG or IgM in different micro-ELISA strip plate respectively and HRP conjugate HTLV antigen appeared blue in colour and then yellow after addition of the stop solution. The optical density (O.D) was measured using a spectrophotometer at a wavelength of 450nm. The presence of anti-HTLV IgG or IgM antibodies in different micro- ELISA strip plate, respectively, was determined by comparing the O.D of sample to CUT OFF value of the plate according to manufacturers’ instruction. The reagents and samples was allowed to reach ambient temperature (25°C) for 30 minutes. Wells was numbered including one Blank, three for the Negative control and two for the positive control. Fifty (50) µl of Positive control, negative control, and test sera was added into their respective wells except the blank. A separate disposal pipette tip was used for each specimen, negative control and positive control to avoid cross-contamination. Fifty (50) µl HRP-Conjugate (Horseradish peroxidase-conjugated anti-HBS) was added to each well except the Blank, and mixed by tapping the plate gently. The plate was covered with plate cover and incubated for 60 minutes at 37°C. Plate cover was removed and discarded. The plate was emptied by aspiration and washed each well 5 times with diluted Wash buffer. After the washing cycle, the plate was dried by turning them upside down onto blotting paper. Fifty (50) µl of chromogen A (Urea peroxide solution) and fifty (50) µl chromogen B (tetramethylbenzidine) was dispensed into each well including the Blank, and mixed by tapping the plate gently. The plate was incubated at 37°C for 15 minutes avoiding light. The enzymetic reaction between the chromogen solutions and HRP-Conjugate produces blue colour in positive control and HTLV 1/2 positive sample well. Multichannel pipette was used to stop the reaction by adding fifty µl stop solution (diluted sulphuric acid solution 0.5 M H2SO4) into each well and was mixed gently. Intensive yellow colour develops in positive control and HTLV 1/2 positive sample wells. The plate reader was calibrated with the blank well and the absorbance was read at 450nm within 15 minute. Specimens giving absorbance less than the cut-off value are negative for this assay, which indicates that no HTLV 1/2 virus surface antigen has been detected with this HTLV 1/2 ELISA. Specimens giving an absorbance equal to or greater than the cut-off value are considered initially reactive, which indicates that HTLV 1/2 virus surface antigen could probably be detected using this HTLV 1/2 ELISA (Nanjing Pars Biochem, China) [9].
Statistical analysis
All generated data was analyzed using SPSS software version 26.0 (2016, IBM California, USA). The prevalence of HTLV-1/2 will be expressed in simple proportions and percentages for the study groups. Chi-square contingency table will be used to determine the relationship between seroprevalence of HTLV-1/-2 infections and HIV in relation to age group, gender and ethnicity. A confidence interval of 95%, p-values <0.05 were considered statistically significant.