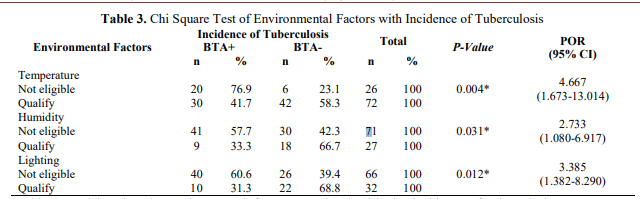
Temperature is associated with the incidence of tuberculosis. The air temperature in the house is said to be ideal if it ranges from 18-30oC. Inappropriate temperatures will potentially lead to conducive bacterial growth and cause health problems such as dehydration. Mycobacterium tuberculosis bacteria can live and grow well at temperatures ranging from 31oC-37oC [8].
Temperature measurements are carried out in the living room where the room is a spacious room where family members gather. This is in accordance with research conducted in Surabaya where home temperature measurements are carried out at the point where family members often gather, including tuberculosis sufferers. Observations in the field showed that respondents with unqualified home temperature had a habit of rarely opening the windows of a house or room. The reason is because many family members do activities outside the home (school / work) so it is not safe if the window of the house is open and some respondents think that opening the window will make dust enter the house. Windows or doors that rarely open cause impaired air circulation [9].
Another study in the United States stated that the average daily minimum temperature (with positive effects) is an important climate factor in. This may be due to the adverse effects of minimum air temperature on the patient's respiratory system, and the lifestyle of people closer in cold weather which increases the risk of exposure to tuberculosis infectious agents [10]. Similar results were reported in other studies. In a time series analysis study in Fukuoka (Japan), Onozuka and Hagihara found a significant positive association between extreme cold temperatures and cases of tuberculosis incidence [11]. Our results are also consistent with findings in Pakistan [12].
Humidity is associated with the incidence of tuberculosis. High humidity is a living place for Mycobacterium tuberculosis bacteria. Ideally a house has humidity ranging from 40-60%. If the air humidity <40% then it is necessary to make an effort to open the ventilation of the house either windows or doors. If the air humidity >60%, then it needs efforts such as installing glass tiles or using a humidifier so that humidity becomes ideal [13].
The results showed that there were respondents who had qualified home humidity but suffered from tuberculosis. According to researchers, someone who has a qualified physical environment condition of the house has more high degrees of health. But good environmental factors are not enough for a person to avoid tuberculosis, the need for the application of healthy behaviors by all family members such as not smoking in the house and consuming a balanced diet so that the body's resistance is strong. The results of observations made by researchers are known that most of the respondents' homes are in densely populated neighborhoods. The houses feel stuffy because many people rarely open windows. The absence of air exchange in the house can trigger high levels of humidity. Unhealthy environmental conditions and high humidity in the house can trigger the fertile growth of tuberculosis-causing bacteria [9].
In our study, the risk of tuberculosis was more in those who lived at home with ineligible inertia. Research in Hong Kong states that a higher risk of tuberculosis notification occurs when relative humidity is 60.0–63.6% [14]. A study in Southwest China revealed that minimum relative humidity correlates inversely with the number of tuberculosis cases [15].
Although moisture inaction was inconsistent among these four studies, these findings suggest that lower humidity levels are closely associated with more cases of tuberculosis with slowness effects of varying lengths. One possible reason for the explanation is that in dry conditions the body's airway mucus secretion and cleansing of exogenous pathogens is reduced, which can make people more susceptible to mycobacterium tuberculosis infection [16].
Lighting is associated with the incidence of tuberculosis. A room ideally has 60 lux of lighting, while for corridors it is at least 20 lux [5]. Lighting should be ideal because sunlight has a role to kill bacteria and other microorganisms, especially those found in the home environment. A humid and dark home environment will make mycobacterium tuberculosis bacteria live and multiply [17].
The results showed that there were respondents who had qualified home lighting but suffered from tuberculosis. According to researchers, someone who has a qualified physical environment condition of the house has more high degrees of health. All family members need to adopt healthy behaviors such as not smoking indoors, applying the correct cough ethics and consuming a balanced diet so that the immune system is strong. The results of observations made by researchers showed that most of the respondents' homes did not have enough natural lighting. This is because the respondent's house is in small alleys where sunlight is blocked by house buildings. Coupled with the habits of people who rarely open windows and doors make the conditions in the house dark and humid.
The results of the above study are in line with other studies that state that most people with pulmonary tuberculosis have poor home lighting. The results of statistical tests showed a significant association between lighting and tuberculosis incidence [18]. Other studies have shown a significant association between lighting and the incidence of tuberculosis, as well as the condition of homes with ineligible lighting 3.5 times the chance of developing tuberculosis [18]