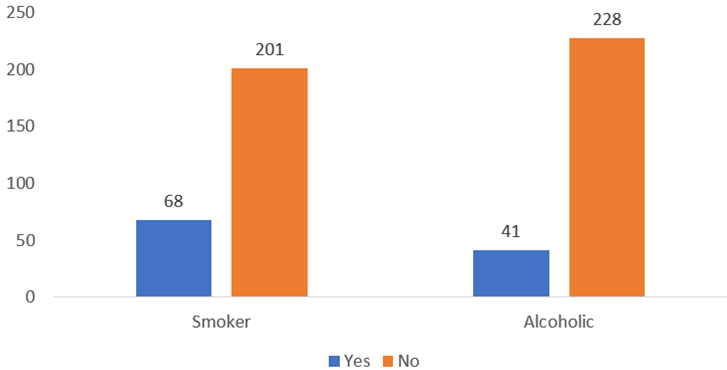
The females were found to be affected more by thrombophlebitis in our study as compared to males. Similar results were found in the study conducted by Singh et al. [6] on 230 patients admitted in the Intensive Care Unit, medical, surgical, obstetrics and gynaecology wards of Dhulikhel Hospital. Salma et al. [7] also found out that the incidence waws higher in the male patients but Comely et al. [8] found that the incidence of thrombophlebitis was more in females, hence this study is in concordance with our findings. In our study, phlebitis was more common in patient group of less than 60 years than the patients above 60 years of age. This result coincides with the result of other studies [7-8]. This may attributed to the fact that as the inflammatory response in the elderly is often impaired, signs and symptoms of phlebitis may be stable.
One of the most striking findings of our study was that phlebitis was found in only 10% of the diabetic patients. This result of our study does not coincide with the result of the study conducted by Salma et al. [7] at Dhaka National Medical College Institute Hospital [7]. In this study, the prevalence of diabetics was 25%. A higher proportion of phlebitis in these patients may be due to the endothelial damage induced by diabetes mellitus, that predisposes patients to phlebitis. Good control of diabetes mellitus, greater attention and care during insertion and changing catheters within 72 hours may reduce the rate of phlebitis in these patients [5].
In our study, there were nearly one-fourth of the study participants who were hypertensive. This is in contrast to the result of the study conducted by Maki et al. [9]. In their study the proportion of patients with HTN was nearly one-third of the study population.
In our study, dyslipidemia was found in approximately 15% of the study particpants. This is similar to the result found in the study done by Monreal et al. [10]. In addition, they also found that the rate of thrombophlebitis was significantly higher in hyperlipidemia group (17.11%) compared to group without hyperlipidemia.
The prevalence of thrombophlebitis was high among the study participants. This is comparable with the other studies [11,12].